Acne Treatment Harley Street, London

Those suffering with acne understand all too well its effects on confidence and self-esteem, but finding a solution that works for you is no easy task. Chopping and changing skincare in hopes of finding a cure, and cutting out large food groups in an attempt to control the skin, are all too common occurrences often leading to frustration, wasted money, and worry around food. It is important to understand the type of acne you suffer from to successfully treat it. After her own well-documented struggles with acne, Self London founder Dr Anjali has a special interest in this field and is one of the UK’s leading experts on acne and its treatment.
Self London has expertise in light and laser-based treatments such as AviClear and BroadBand Light. AviClear is the world’s first and only FDA-approved treatment for the management of mild, moderate and severe acne which is safe across all skin types. It is also highly effective, with outcomes comparable to oral medications. Having multiple options for acne management is central to providing a comprehensive and well-led service, and this is exactly what Self London does well.
Book your consultation today at our medical dermatologist clinic on Harley Street to discuss the best acne treatment for you.
What is acne?
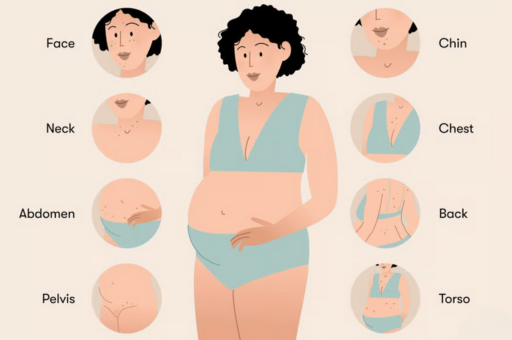
Acne vulgaris is a chronic skin condition caused by blockage or inflammation of the hair follicles and their associated sebaceous glands. It typically affects areas with the highest density of oil glands; this includes the face, upper chest and back. Although all age groups can be affected, it usually starts in adolescence. It can present as non-inflammatory comedones (blackheads, whiteheads), inflammatory papules, pustules, nodules and cysts, or a mixture of lesions. This can result in symptoms of local pain and redness.
Acne is extremely common and thought to affect most people at some point in their lives. 20% progress to severe acne, which can lead to permanent acne scarring. The condition can be associated with significant psychosocial complications including low self-esteem, altered body image, social isolation and depression. The aims of treatment are to prevent long-term complications.
What causes acne?
Acne develops from a complex interplay between multiple factors. Genetics are thought to play an important role, as the number and size of sebaceous glands and their activity are inherited. Twin studies show that the concordance rate for the prevalence and severity of acne is extremely high. The heritability of acne is almost 80% in first-degree relatives.
Oil gland activity is under the influence of hormones, in particular the androgen dihydrotestosterone. During adolescence, the body produces androgen hormones from the reproductive organs and adrenal glands. These hormones act directly on the sebaceous gland to increase oil production and excretion. Increased sebum combined with abnormal follicular hyperkeratinisation results in “sticky” skin cells or keratinocytes blocking the pilosebaceous duct, and subsequent blocking of pores. Bacteria that naturally live on the skin forming part of the skin microbiome can then stimulate inflammation, causing deeper acne lesions.
What does acne look like?
Acne is characterised by comedones, papules, pustules, nodules and cysts:
- Comedones are the most basic acne lesions and can be open or closed. Closed comedones (whiteheads) are small, plugged follicles whose contents are not exposed to the skin surface. Open comedones (blackheads) are small follicles with dilated openings on the skin. The black colour results from oxidation of the debris within the follicle.
- Papules are small, usually red, raised elevations of the skin.
- Pustules resemble papules but have a central pocket of pus.
- Nodules and cysts are larger painful swellings, usually >5mm in size.
Examination of the skin sometimes reveals other lesions that have developed as a consequence of the acne. These include atrophic or pitted/indented scars, post-inflammatory erythema (redness) or hyperpigmentation (dark staining), and keloids. The latter two are more common with darker skin.
How can you treat acne?
Topical treatments
Retinoids: These agents are derived from vitamin A. They correct abnormal follicular hyperkeratinisation and inhibit new comedone formation. The most commonly used topical retinoids include tretinoin and adapalene. Skin irritation and redness can occur in the early phase of treatment. These agents thin the upper barrier layer of the skin (stratum corneum) and can increase photosensitivity; sun protection is therefore important alongside this treatment.
Benzoyl peroxide: Benzoyl peroxide is a bactericidal agent with the ability to reduce C. acnes numbers around the oil gland. It is useful for both inflammatory and non-inflammatory acne lesions, and is not associated with bacterial resistance. Products containing benzoyl peroxide are available over the counter or by prescription, and are used once or twice daily.
Antibiotics: Topical antibiotics, commonly clindamycin, are often used for their activity against C. acnes. There is a risk of bacterial resistance with these agents so they are not used alone and are usually combined with either retinoids or benzoyl peroxide. Topical antibiotic usage should, if possible, be limited to no more than 12 weeks.
Azelaic acid: This can be used as a second-line option for acne if other treatments are unsuitable or not tolerated. There is less scientific data on this agent, and results are mixed. It can, however, have a beneficial role in the right patient after proper consultation.
Oral treatments
Antibiotics: These have anti-inflammatory properties and activity against C. acnes. Oral antibiotics can be successfully combined with topical retinoids or benzoyl peroxide in moderate acne. First-line agents include tetracycline, oxytetracycline, doxycycline and lymecycline. There is good evidence that these agents can reduce inflammatory lesion counts and severity. Other antibiotics used include erythromycin, azithromycin and trimethoprim. Tetracycline antibiotics should not be used during pregnancy, but erythromycin is a safe alternative in this situation. Average treatment time is about 12 weeks.
Hormonal therapies: The combined oral contraceptive pill can be used to control acne in women requiring contraception. Oestrogen in the contraceptive pill reduces sebum production. It also reduces ovarian production of androgens and can have actions on the liver which result in an overall reduction of free testosterone. These can all be of benefit to female patients suffering with acne.
Spironolactone can be used by consultant dermatologists in the treatment of acne. It has a number of anti-androgenic properties (it reduces androgen hormones). Spironolactone has a useful role against acne in adult women and in the context of PCOS. It is an unlicensed medication for the management of acne in the UK and should only be prescribed by specialists who have experience in its use.
Isotretinoin: Isotretinoin is a systemic retinoid that is highly effective in severe acne vulgaris. It also has a role in acne that is scarring, fails to respond to treatment with other agents, relapses quickly after completion of antibiotic therapy, or has a profound psychological impact. In the UK, it should only be prescribed under the supervision of a dermatologist as it requires careful monitoring.
There have also been reported and well-publicised cases of mood disorders in association with isotretinoin. Although no clear cause-and-effect relationship has been definitively established, patients should be warned of this potential link.
Light and laser acne treatments
There are some patients for whom oral medication is not an option. This may be personal preference, because they are trying to conceive or undergoing fertility treatment, or because they are otherwise unsuitable for other medical reasons. Self London has expertise in light- and laser-based treatments such as AviClear and BroadBand Light. AviClear is a revolutionary new acne treatment with excellent and long-lasting outcomes comparable to those of oral medications. Offering multiple options is central to providing a comprehensive, well-led acne service, and this is exactly what Self London does well.
Steroid injections
Intralesional corticosteroid injections: Steroid injections can be used in clinic by a dermatologist to flatten acne nodules or cysts quickly (eg, before a special event). Injections can be useful for isolated cysts where a quick response is required and should only be performed by a specialist as there are several potential side-effects, including atrophy (indented scar) and infection.
For more information and support on acne and acne scarring, visit the British Association of Dermatologists acne support website. Self London founder, Dr Anjali, was a key contributor in its development, content and peer review process.
For expert help with your acne, contact the clinic to book a consultation.